Back Pain That Doesn’t Go Away? It Could Be Bertolotti Syndrome
Chronic lower back pain, also traditionally known as lumbago, is one of the most common reasons people seek medical attention. Yet for many patients, the underlying cause is not always straightforward. In some cases, especially in younger individuals or those who’ve seen multiple specialists without progress, the problem may stem from a structural issue that has been overlooked. This is where Bertolotti Syndrome comes in.
Also referred to as Bertolotti disease, this condition is often missed in routine assessments and can lead to persistent pain, restricted mobility, and failed conservative treatments. But with the right diagnosis and a minimally invasive surgical approach, patients can experience life-changing results, improving their long-term quality of life.
What Is Bertolotti Syndrome?
Bertolotti Syndrome is a congenital spinal condition where the lowest lumbar spine vertebra (L5) forms an abnormal connection (called a lumbosacral transitional vertebra) with either the sacrum or iliac bone. In simpler terms, the bottom vertebra may be partially fused or connected in a way that alters how the spine moves. This creates usually unilateral low back pain, due to uneven stress distribution across the lower spine, often affecting soft tissues around the joint.
This structural anomaly can cause:
Localised low back pain, usually on one side
Sciatica-type symptoms
Leg pain with sitting, standing, or walking for long periods
Poor response to standard physical therapy
Because it’s relatively rare and frequently overseen on basic X-rays, MRI’s, Bertolotti Syndrome is often misdiagnosed or missed altogether.
Advanced Imaging: Unlocking the Real Cause
In this case, the patient underwent a full diagnostic work-up, including:
MRI imaging, ruling out disc changes and possible nerve compression
CT scan, used to properly visualise bony anatomy and see how big is connection of the transverse process with the sacrum and if there is any evidence of arthritis
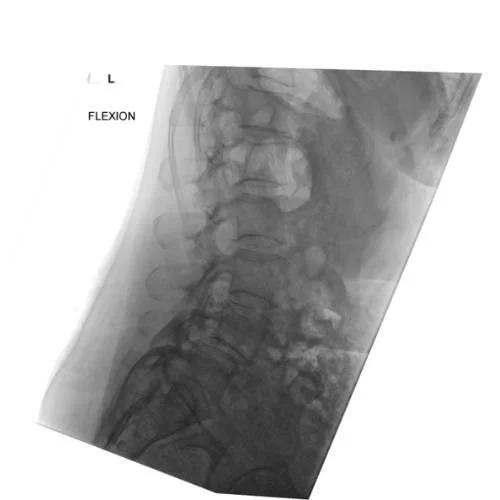
Dynamic flexion X-ray, to assess spinal movement and stability, a critical tool in evaluating if there is no instability in the spine.
These tools enabled a precise diagnosis, ruling out “non-specific” mechanical pain and identifying Bertolotti Syndrome as the root cause, allowing for better treatment options.
Conservative Management as First-line for management of Bertolotti Syndrome
Most patients will respond to non-operative measures:
Activity modification
Avoid activities that exacerbate pain (prolonged standing, heavy lifting, flexing, bending).
Pharmacologic therapy
NSAIDs or acetaminophen for pain relief.
Muscle relaxants for spasm.
Short course of neuropathic pain medications (e.g., gabapentin) if a patient has radicular pain.
Physical therapy
Core strengthening and flexibility exercises with postural correction.
Exercise that will increase lumbosacral mobility.
Interventional pain management
Local anaesthetic ± corticosteroid injections into the pseudo-articulation. Injection will be diagnostic and therapeutic at the same time, because it will confirm if the pain is originating fro pseudo joint.
Radiofrequency ablation (RFA) of the pseudo-articulation to provide longer-term relief in selected patients who had successful pain relief after injection and in whom pain returned. RFA will try to make it go away for a longer period of time and try to avoid patients going for surgical intervention.
Surgical Management (for refractory cases) When Conservative Management Fails
Surgery is reserved for patients with persistent pain despite exhaustive conservative therapy and with imaging evidence correlating the transitional segment to symptoms.
Surgical options include:
Resection of the pseudo-articulation (“Processectomy”)
Removal of the anomalous transverse process or pseudo-joint to eliminate abnormal articulation via open or minimal invasive approach
Indicated when pain is clearly localised to the pseudo-articulation and not associated with instability that can occur in some cases
Surgical resection provides good pain relief in well-selected cases, that is successful in more than 90% of the cases.
Spinal Fusion (might be the right choice) if There is Evidence of Segmental Instability
Once segmental instability is diagnosed, the patient might be offered a Minimally Invasive Transforaminal Lumbar Interbody Fusion (MIS TLIF). This surgical technique allows the surgeon to:
Access the damaged disc and compressed nerves with a small incision
Remove the problematic disc
Insert a cage and bone graft to stabilise the segment
Use screws and rods to support proper spinal alignment
Unlike open surgery, MIS TLIF reduces tissue trauma, blood loss, infection rate, hospital stay, and recovery time, while offering the same long term benefits in terms of pain relief and spinal support.
MIS TLIF is also commonly used to treat other causes of back and leg pain, particularly in patients with underlying structural or degenerative spinal conditions. These include:
Degenerative disc disease – when the discs between vertebrae lose height and cushioning ability, and there is foraminal stenosis causing nerve root impingement
Spondylolisthesis – when one vertebra slips forward or backward over the one below it, and there is instability on flexion/extension or standing x ray of the lumbar spine
Spinal stenosis – a narrowing of the spinal canal that can compress the spinal cord or nerve roots, and patient had previous decompression or multiple discectomy on the same level.
In these cases, MIS TLIF offers a targeted approach to relieve nerve root pressure, restore spinal alignment, making it a valuable option for a range of patients beyond those with Bertolotti Syndrome.
Recovery and Outcome
While outcomes will vary depending on the individual's condition and surgical complexity, a typical recovery timeline after MIS TLIF looks like this:
Immediate Post-Operative Phase (0–2 Days)
Patients are usually up and walking within 24 hours post-surgery.
Hospital stay is typically 2-3 nights, significantly shorter than traditional open surgery.
Pain is managed with a combination of analgesics, ice pack and early mobility is encouraged to reduce the risk of complications such as blood clots.
Early Recovery (First 2–6 Weeks)
Most patients return home with a structured care plan, including post-operative instructions of increased mobility in the first weeks after operation.
Driving, lifting,bending, twisting and prolonged sitting may be restricted during this time.
Walking and light daily activities are usually encouraged to support healing and prevent stiffness.
Intermediate Recovery (6–12 Weeks)
Physical therapy is often ramped up to include core strengthening and flexibility exercises, when pain and discomfort improved.
Many patients begin returning to light work duties or part-time routines, depending on the nature of their job.
Pain levels typically continue to decline, with reduced reliance on medication.
Long-Term Recovery (3–6 Months and Beyond)
Full fusion of the operated spinal segment can take up to 12-24 months, which can be sped up with the use of the bone morphogenetic protein type 2 (InductOS) in less then 6 months time.
Most individuals regain substantial improvement in mobility, stability, and pain reduction by the 3–6 month mark. Activities such as low-impact sports, driving, and travel may be resumed with guidance from the surgical team, depending on the bone quality, fusion at 6 months mark and expected level of the physical activity.
Ongoing focus on postural awareness, core strength, and avoiding high-impact strain is key to maintaining long-term results in the first 6 months after surgery.
What to Expect Over Time
Reduced nerve-related pain (e.g. leg pain, sciatica, or tingling) as decompression settles.
Improved sleep, ability to work, and return to daily activities.
A return to being physically active with appropriate adjustments to protect the spine.
MIS TLIF is designed to minimise disruption to soft tissues, reduce blood loss, and promote faster healing, making it an excellent option for patients seeking a quicker return to normal life compared to traditional open surgery.
Cast Study: Bertolotti Syndrome Treated with MIS TLIF
Imaging is essential in diagnosing and planning treatment for Bertolotti Syndrome. In this case, advanced imaging was used to confirm the diagnosis and guide the surgical approach:
Pre-operative MRI: Shows narrowing around the lumbar spine and nerve roots, helping identify the cause of persistent back and leg pain.
Dynamic X-ray: Taken in flexion to assess spinal movement and check for instability. This helped confirm that surgery was necessary to stabilise the segment.
Post-operative CT scan : Demonstrates the placement of screws and rods following a Minimally Invasive Transforaminal Lumbar Interbody Fusion (MIS TLIF). This confirms the stability of the operated level and successful alignment of the spine.
By combining these imaging tools, the surgical team was able to make a precise diagnosis and ensure a stable outcome. The patient went on to achieve significant pain relief and restored mobility in the months following surgery.
The Importance of Specialist-Led Diagnosis
Many individuals live with back pain for years without a clear diagnosis. Often, they receive generic treatments like pain relief, physical therapy, or even injections that don’t target the true issue. That’s why working with a spine surgeon with complex surgical expertise is so important.
Mr Gordan Grahovac regularly treats patients with uncommon or complex spinal conditions such as Bertolotti Syndrome. His multidisciplinary approach combines orthopaedic precision with neurological insight, ensuring no important detail is missed, even in conditions that affect facet joints or soft tissues. He works closely with neuroradiologists with special interest in complex spine disease.
Could Your Back Pain Be Something More?
If you’ve experienced chronic low back pain that hasn’t improved with conservative care, and especially if symptoms radiate into the leg or worsen with movement, it’s worth seeking expert evaluation. Bertolotti Syndrome is just one of many treatable causes of complex spinal pain.
Understanding the risk factors, having access to the right treatment options, and involving a specialist who understands what is causing your pain and discomfort are essential steps to quick solution of your problems.
Early diagnosis can lead to better outcomes and prevent years of unnecessary discomfort.
Book a Consultation
Mr Grahovac is one of the UK’s leading spine surgeons in London and Kent, and sees patients from across the UK seeking back pain treatment and permanent pain relief. He has specialist expertise in Bertolotti Syndrome, spinal stenosis, spondylolisthes, csf leaks, and more.
Take the first step toward understanding your pain and getting the right care. Book a consultation today.